Pain Relief Medicines
-

-
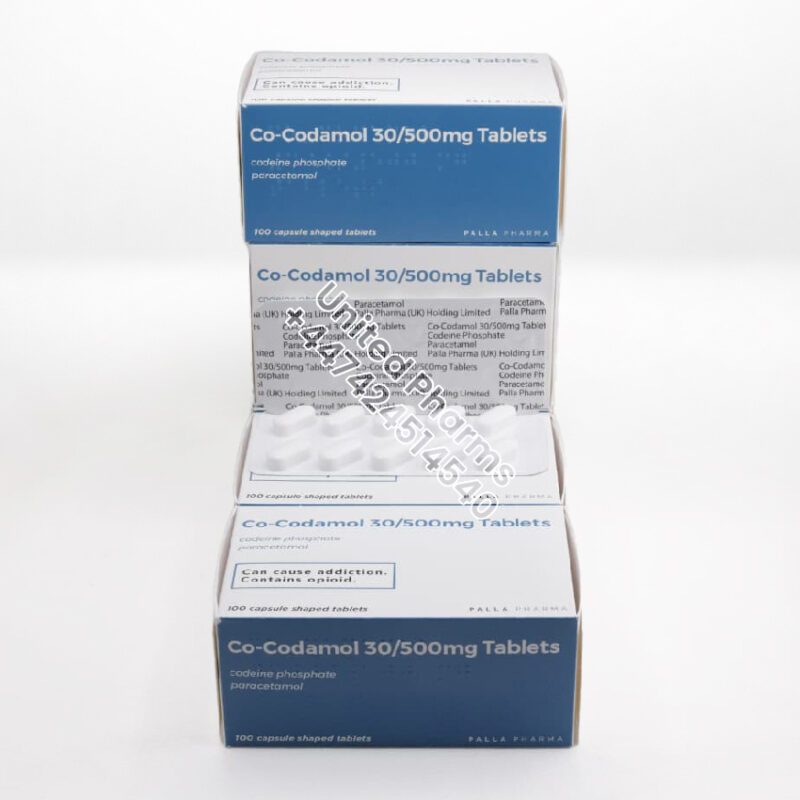
Co-codamol 30/500mg | Palla Pharma – (100 Tablets)
£89.99Original price was: £89.99.£69.99Current price is: £69.99. -

Co-codamol 30/500mg Tablets | Zentiva – (100 Tablets)
£89.99Original price was: £89.99.£69.99Current price is: £69.99. -
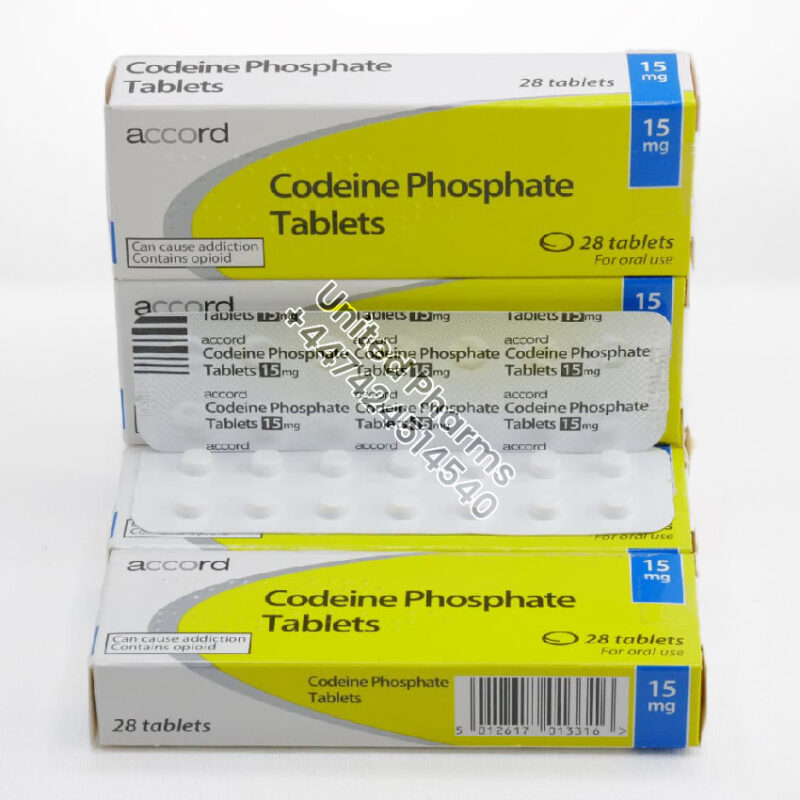
Codeine Phosphate 15mg | Accord – (28 Tablets)
£49.99Original price was: £49.99.£21.99Current price is: £21.99. -
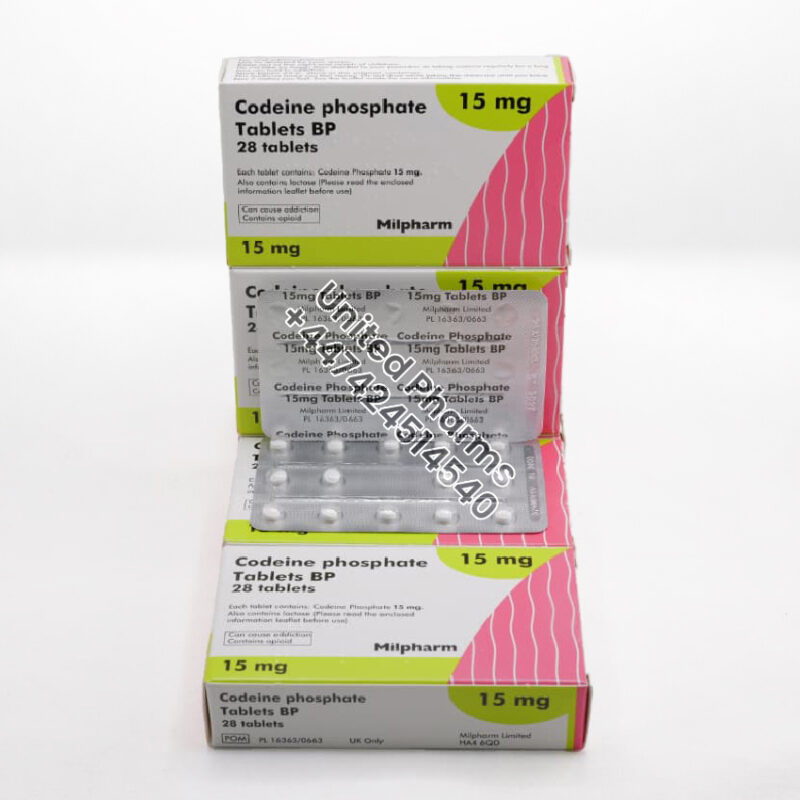
Codeine Phosphate 15mg | Milpharm – (28 Tablets)
£39.99Original price was: £39.99.£20.99Current price is: £20.99. -
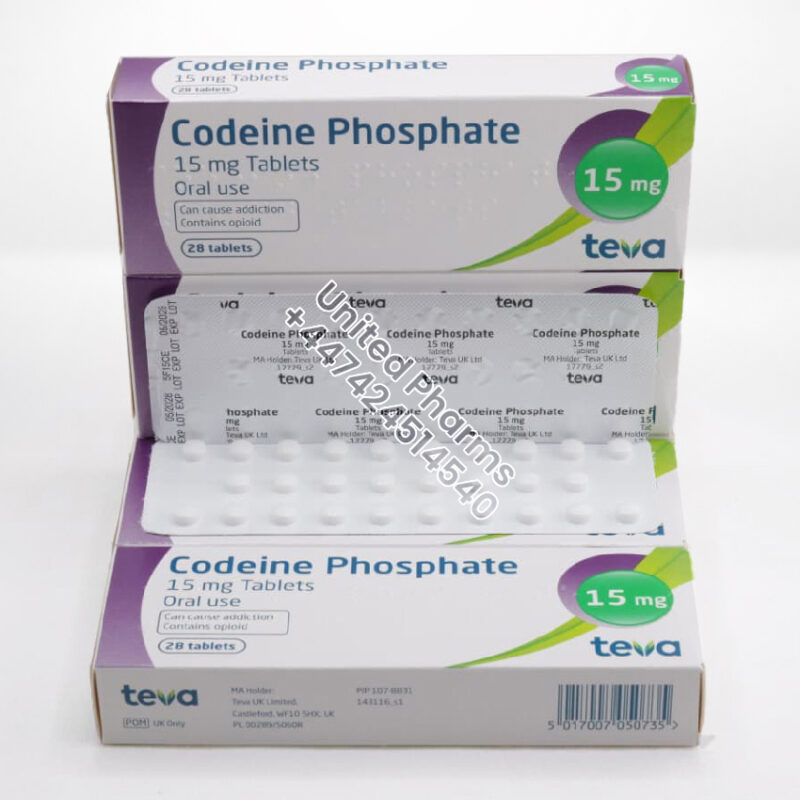
Codeine Phosphate 15mg | Teva – (28 Tablets)
£39.99Original price was: £39.99.£20.99Current price is: £20.99. -
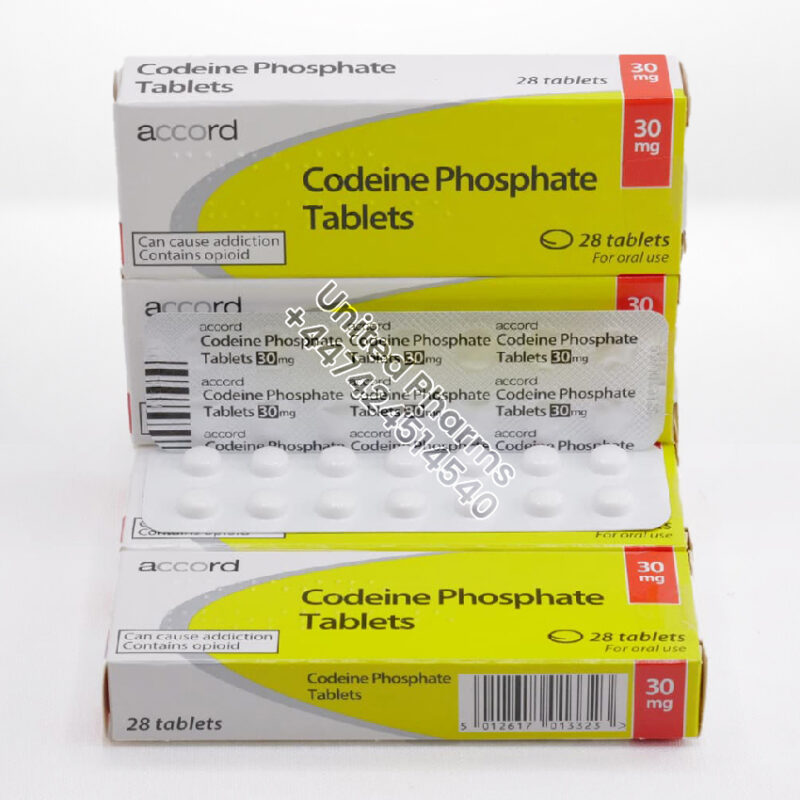
Codeine Phosphate 30mg | Accord – (28 Tablets)
£89.99Original price was: £89.99.£44.99Current price is: £44.99. -
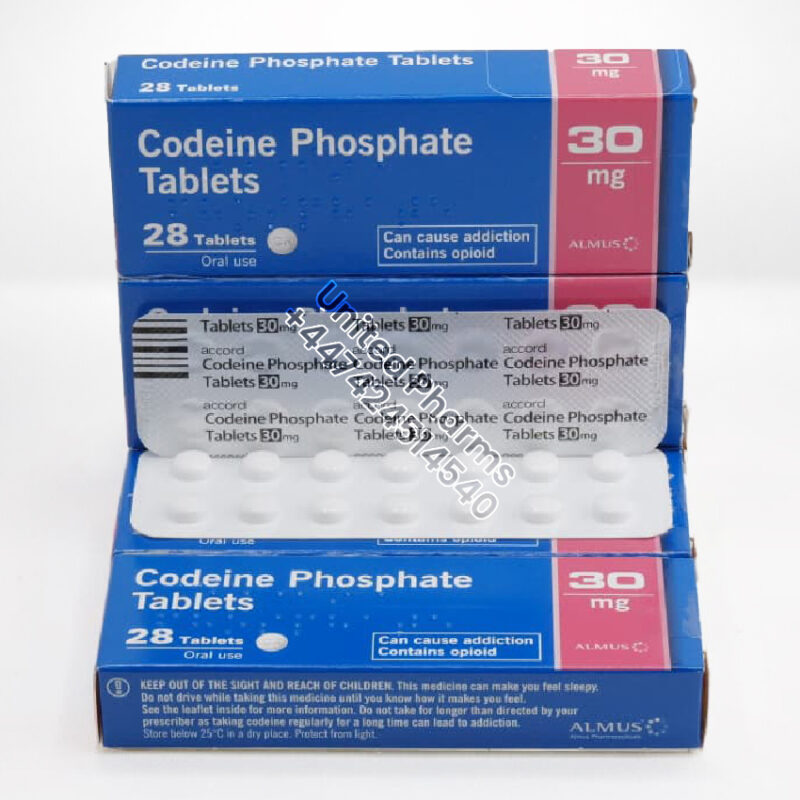
Codeine Phosphate 30mg | Almus – (28 Tablets)
£89.99Original price was: £89.99.£44.99Current price is: £44.99. -
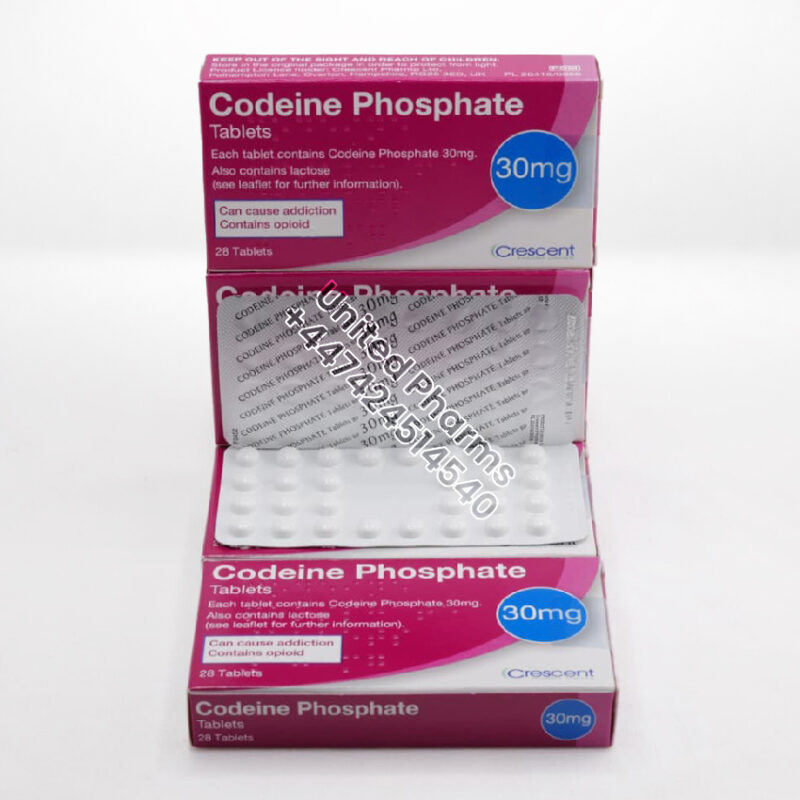
Codeine Phosphate 30mg | Crescent – (28 Tablets)
£89.99Original price was: £89.99.£44.99Current price is: £44.99. -
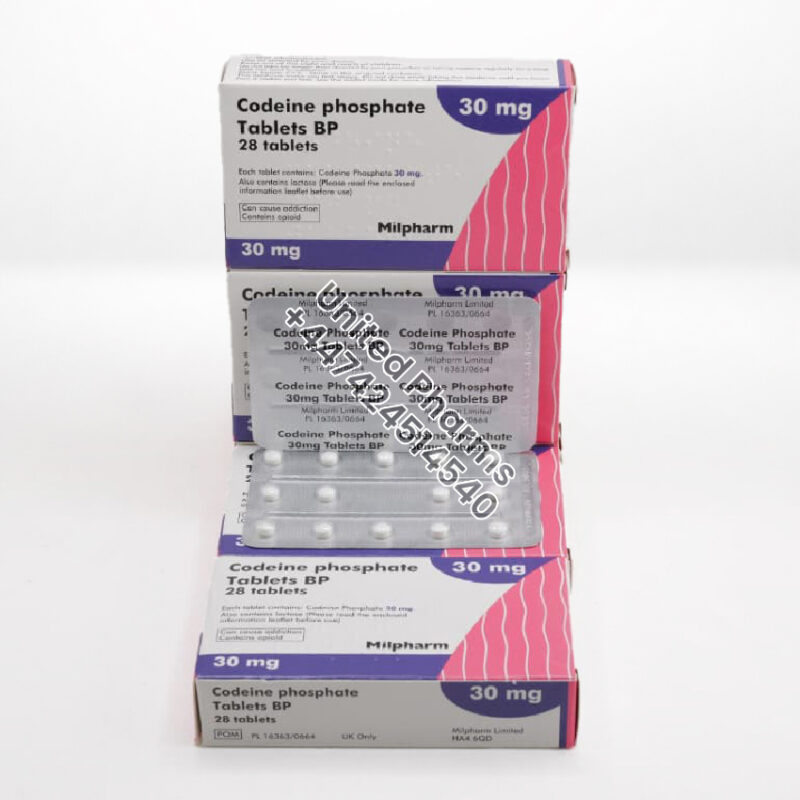
Codeine Phosphate 30mg | Milpharm – (28 Tablets)
£89.99Original price was: £89.99.£44.99Current price is: £44.99. -

Codeine Phosphate 30mg | Teva – (100 Tablets)
£150.00Original price was: £150.00.£129.99Current price is: £129.99. -

Codeine Phosphate 30mg | Teva – (28 Tablets)
£89.99Original price was: £89.99.£44.99Current price is: £44.99. -
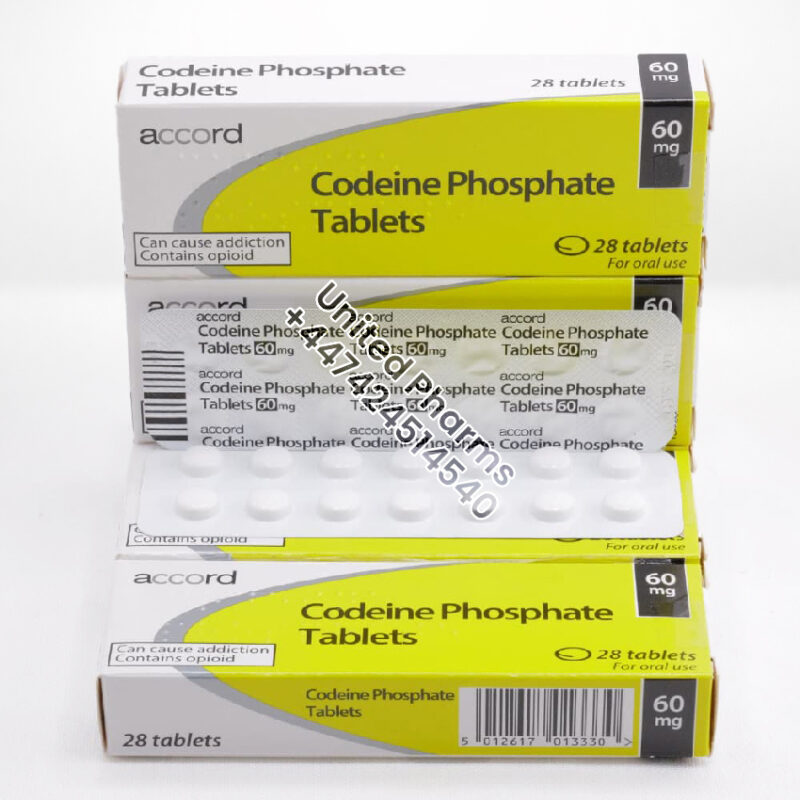
Codeine Phosphate 60mg | Accord – (28 Tablets)
£89.99Original price was: £89.99.£74.99Current price is: £74.99. -
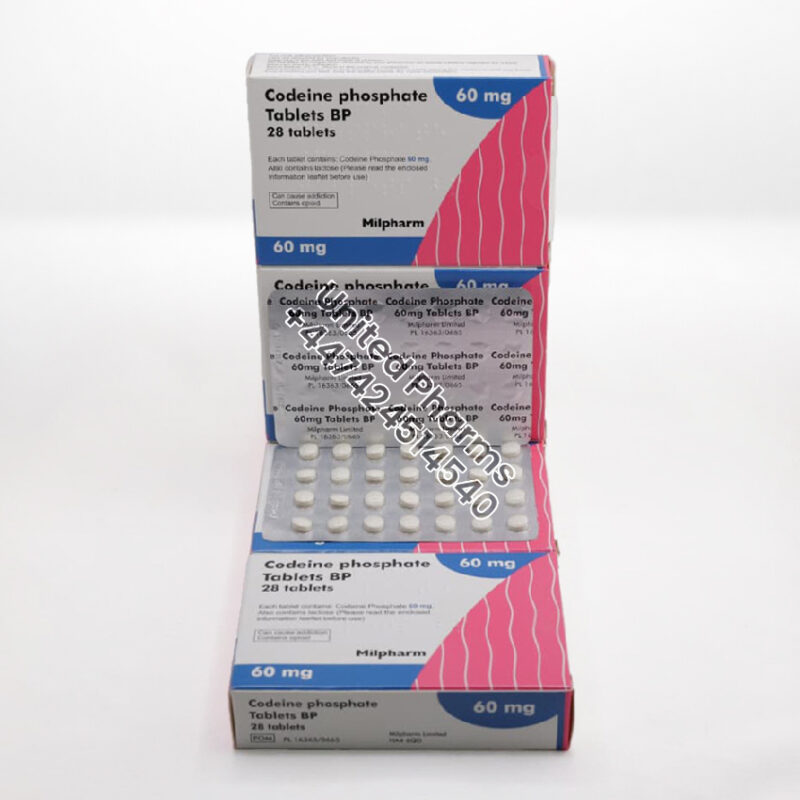
Codeine Phosphate 60mg | Milpharm – (28 Tablets)
£119.99Original price was: £119.99.£74.99Current price is: £74.99. -

Dihydrocodeine Continus 60mg | Napp Pharma – (56 Tablets)
£189.99Original price was: £189.99.£139.99Current price is: £139.99. -
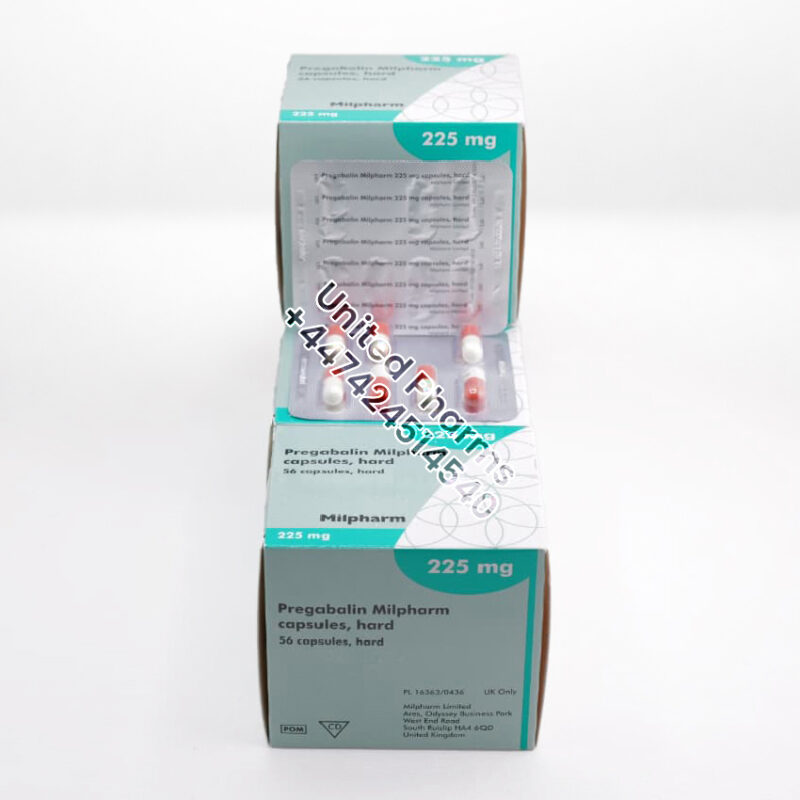
Pregabalin 225mg | Milpharm – (56 Capsules)
£69.99Original price was: £69.99.£49.99Current price is: £49.99.
End of content
End of content
Pain Relief Medicines – Buy Online in UK /
Pain relief medicines (analgesics) are a group of prescription treatments used to manage acute, chronic, and neuropathic pain. They help reduce discomfort, improve mobility, and support day-to-day functioning when pain significantly affects quality of life. This category includes widely used medicines such as Co-Codamol, Codeine Phosphate, Dihydrocodeine, Pregabalin, Tramadol Hydrochloride, and other clinically recognised treatments.
These medicines work through various mechanisms—some act on the central nervous system to modify pain signals, while others help regulate nerve activity. Many are controlled medicines in the UK, requiring proper clinical assessment and safe-use guidance.
What These Medicines Are Used For
Pain relief medicines in this category may be prescribed for:
-
Moderate to severe acute pain
-
Chronic musculoskeletal pain
-
Post-operative pain
-
Nerve pain (neuropathic pain)
-
Sciatica and nerve compression
-
Pain linked with injury or inflammation
-
Pain that has not responded to non-opioid analgesics
-
Mixed pain conditions where nerve and tissue pain coexist
How These Medicines Work
Different medicines provide pain relief through different pathways:
Opioid & Opioid-Based Analgesics (e.g., Co-Codamol, Codeine, Dihydrocodeine, Tramadol)
-
Bind to opioid receptors in the brain and spinal cord
-
Reduce pain perception
-
Useful for moderate to severe pain
-
Often used when paracetamol or NSAIDs are insufficient
Gabapentinoids (e.g., Pregabalin)
-
Act on calcium channels in nerve cells
-
Reduce abnormal nerve signalling
-
Effective for neuropathic pain and fibromyalgia
-
May be used long-term under supervision
Combination Medicines (e.g., Co-Codamol)
-
Combine opioid + paracetamol for enhanced pain control
Common Benefits
-
Effective management of moderate to severe pain
-
Improvement in mobility, sleep quality, and daily functioning
-
Targeted options for nerve pain and mixed pain conditions
-
Multiple formulations available (capsules, tablets, soluble, prolonged-release)
-
Can be used short-term or long-term depending on clinical need
Limitations & Considerations
-
Some medicines (especially opioid-based) may cause dependence, tolerance, or withdrawal
-
Risk of drowsiness, dizziness, or reduced coordination
-
Potential interactions with alcohol, sedatives, and other medicines
-
Not suitable for all patients, including those with certain respiratory or liver conditions
-
Long-term use should be regularly reviewed
-
May affect ability to drive or operate machinery
Possible Side Effects
Common
-
Drowsiness
-
Nausea
-
Constipation
-
Dizziness
-
Dry mouth
-
Headache
Occasional
-
Mood changes
-
Sleepiness
-
Reduced alertness
-
Sweating
-
Itching
Rare but Serious
-
Breathing difficulties
-
Severe allergic reactions
-
Confusion or agitation
-
Misuse or dependence
-
Withdrawal symptoms if stopped abruptly
Seek immediate help if serious reactions occur.
When Not to Use These Medicines
Avoid use unless evaluated by a clinician if you have:
-
Severe respiratory disease
-
Sleep apnoea
-
History of substance misuse or opioid dependency
-
Severe liver or kidney problems
-
Allergic reactions to opioid-based medicines
-
Pregnancy or breastfeeding (unless specifically approved)
Avoid combining with:
-
Alcohol
-
Benzodiazepines and sedatives
-
Other opioid medicines
-
Strong CNS depressants
UK & EU Examples of Medicines in This Category
These medicines are supplied by multiple established pharmaceutical companies.
Opioid & Combination Analgesics
-
Co-Codamol – Accord, Teva, Kent Pharma, Wockhardt, AAH
-
Codeine Phosphate – TEVA, Accord, Mylan, Aurobindo
-
Dihydrocodeine – Mylan, Teva, Wockhardt, Martindale
-
Tramadol Hydrochloride – Grünenthal (originator), Teva, Actavis, Accord
Neuropathic Pain Treatments
-
Pregabalin – Pfizer (Lyrica), Accord, Teva, Viatris
-
Gabapentin – Teva, Zentiva, Mylan, Accord
These medicines are available in a range of strengths and formulations depending on the clinical requirement.
Frequently Asked Questions (FAQ)
1. Which pain relief medicine is strongest?
This varies by condition. Opioid-based medicines tend to be stronger, while gabapentinoids target nerve pain more effectively.
2. Can I drive while taking these medicines?
Some pain medicines can impair alertness or reaction time. Always check individual guidance before driving.
3. Are these medicines addictive?
Opioids can cause dependence if used long-term. Gabapentinoids may also cause withdrawal symptoms if stopped suddenly.
4. Can I take them with alcohol?
No. Alcohol increases sedation and respiratory risks.
5. Are they safe for long-term use?
Long-term use requires regular medical review to assess benefits, risks, and side effects.
6. Do these medicines treat all types of pain?
No. Some work best for nerve pain (Pregabalin, Gabapentin), while others target moderate to severe physical pain (Codeine, Tramadol).
Conclusion
Pain relief medicines play a crucial role in managing both acute and chronic pain when simpler treatments are not enough. From opioid-based options like Co-Codamol, Codeine Phosphate, Dihydrocodeine and Tramadol to nerve-targeting treatments like Pregabalin, these medicines help reduce pain intensity, support mobility, and improve overall quality of life. As controlled medicines in the UK, they require careful monitoring to ensure safe and effective use. When prescribed responsibly and reviewed regularly, they remain essential tools in modern pain management across UK and EU healthcare systems.
